Disordered eating in high performance sport
The Australian Institute of Sport (AIS) mission is to lead and enable a united high performance (HP) system that supports Australian athletes/teams to achieve podium success.
Disordered eating can occur in any athlete, in any sport, at any time, crossing boundaries of gender, age, body size, culture, socio-economic background, athletic calibre and ability.
The Australian Institute of Sport supports the early identification and prevention of disordered eating in athletes within the high performance sporting system.
Disordered eating (DE) and eating disorders (EDs) are complex and can affect the health (mental and physical) and performance of athletes. The AIS has partnered with the National Eating Disorders Collaboration (NEDC) to produce a position statement to assist sporting organisations to address this serious, but often misunderstood area.
There is a spectrum of eating behaviours in high performance sport that spans from optimised nutrition through disordered eating to clinically diagnosed eating disorders.
The Australian Institute of Sport (AIS) and National Eating Disorders Collaboration (NEDC) position statement on disordered eating in high performance sport.
The AIS partnered with the NEDC and produced a position statement to assist sporting organisations to address this serious, but often misunderstood area. The guidelines are for athletes, coaches, support staff, clinicians and sporting organisations.
The position statement is a call to action to all involved in sport to be aware of poor self-image and poor body image among athletes. The guidelines support the prevention and recognition of disordered eating and promote early intervention to optimise nutrition for performance in a safe, supported, purposeful and individualised manner.
Download Disordered Eating Position Statement
- Disordered Eating Position Statement[PDF • 710.01 kb]
Question and answer with AIS Chief Medical Officer, Dr David Hughes.
Signs and symptoms
Everyone in the sport system has a role to play in recognition and early intervention (‘early identifiers’), and anyone can refer athletes to, and/or consult with, any member of the core multidisciplinary team (doctor, sports dietitian and psychologist) for further assessment and support. Rapport between the athlete and his or her support network (coach, training partners or teammates, service providers) is important in recognising and evaluating DE and EDs.
It is important for all personnel involved in the sport to be aware of the risk factors and warning signs or red flags of DE and EDs and to be informed of effective communication channels for concerns. Some warning signs can occur early (behavioural changes) whereas others such as weight changes may occur later in the person’s trajectory of DE.
Behavioural changes
- Preoccupation with food, calories, body shape and weight
- Polarised/dichotomous thinking (including but not limited to thoughts about food, body or exercise)
- Avoidance of food-related social activities
- Restrictive eating e.g. cutting down or cutting out food groups, nutrients, reducing overall energy intake, counting, measuring and weighing food
- Bathroom visits after meals
- Evidence of binge eating (large amounts of food purchased/consumed, evidence of food wrappers hidden in the bin or another location)
- Restriction followed by binge eating
- Secretive behaviour regarding food intake and/or exercise behaviour
- Increasing rigid or inflexibility in situations
Physical changes
- Wearing baggy or layered clothing that hides body shape
- Relentless, excessive exercise
- Exercise through injury/illness with inadequate recovery
- Bone stress injury
- Hormone dysfunction (including dysregulated menstrual cycle, libido and erectile function)
- Frequent illness
- Low body fat
- Dehydration
- Bad breath, sore gums or signs of enamel loss on teeth
- Swelling around jaw
- Skin effects, including dry skin, fine hairs growing around the face, or signs of calluses on the knuckles
- Unexpected weight gain beyond that expected from growth/development/puberty
- Dramatic or rapid weight loss or gain or fluctuation
Psychological changes
- Persistent and/or declining mental health
- Increased attention to and/or criticism of one’s body
- Feeling out of control with regard to food
- Body image dissatisfaction and distortion
Personal attributes which underpin successful performance, combined with the sport environment, may leave athletes vulnerable to disordered eating.
Common questions
DE may range from what is commonly perceived as normal dieting to reflecting some of the same behaviour as those with eating disorders, but at a lesser frequency or lower level of severity.
DE in an athlete sits on a spectrum between optimised nutrition and an ED, and may include some of the criteria for diagnosis of an ED. Both DE and dieting behaviour are common indicators for developing an ED.
Spectrum of eating behaviour
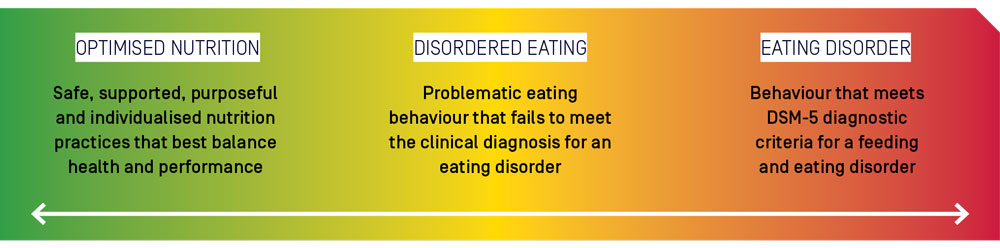
Optimised nutrition - Safe, supported, purposeful and individualised nutrition practices that best balance health and performance
Disordered eating - Problematic eating behaviour that fails to meet the clinical diagnosis for an eating disorder
Eating disorder - Behaviour that meets DSM-5 diagnostic criteria for a feeding and eating disorder
The 2019 International Olympic Committee (IOC) consensus statement on mental health in elite sport compares characteristics of ED versus DE (Reardon et al. 2019)
Eating disorders | Disordered eating |
|---|---|
Restricting, bingeing or purging often occur multiple times per week | Pathogenic behaviours used to control weight (e.g. occasional restricting, use of diet pills, bingeing, purging or use of saunas or ‘sweat runs’) may occur but not with regularity |
Obsessions with thoughts of food and eating occur much of the time | Thoughts of food and eating do not occupy most of the day |
Eating patterns and obsessions preclude normal functioning in life activities | Functioning usually remains intact |
Preoccupation with ‘healthy eating’ leads to significant dietary restriction | There may be preoccupation with ‘healthy eating’ or significant attention to caloric or nutritional parameters of most foods eaten but intake remains acceptable |
Excessive exercise beyond that recommended by coaches may be explicitly used as a frequent means of purging carbs | While exercise may not be regularly used in excessive amount to purge calories, there may be a cognitive focus on burning calories when exercising |
Individual athletes can move back and forth along the spectrum of eating behaviour at any point in time over their career and within different stages of a training cycle (e.g. during the off-season, pre-season, when injured). Athletes are more likely to present with DE than a clinical ED, however, there are health and performance implications regardless of where an athlete falls along the spectrum, as risks increase when DE worsens into a diagnosable ED.
Behaviour that was previously ‘encouraged and rewarded’ such as losing weight to enhance performance, may result in a failure to maintain adequate energy availability required for training and competition demands. These behaviours may not have been maladaptive at first, but may develop into problematic eating behaviour and worsen to reflect ED psychopathology.
Familiarisation with ED diagnostic criteria among members of an athlete’s support network facilitates appropriate questions about eating behaviour. Feeding and eating-related disorders are defined by specific criteria published in the American Psychiatric Association’s (2013) Diagnostic and Statistical Manual of Mental Disorders (5th edition, DSM-5).
Disordered eating and low energy availability can occur together, or in isolation. Identification of one necessitates the investigation of the other.
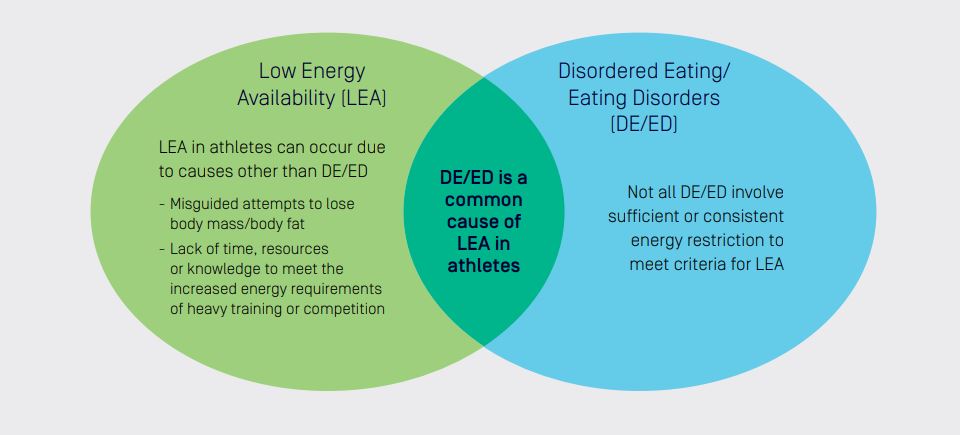
Low Energy Availability (LEA) - LEA in athletes can occur due to causes other than DE/ED
- Misguided attempts to lose body mass/body fat
- Lack of time, resources or knowledge to meet the increased energy requirements of heavy training or competition
DE/ED is a common cause of LEA in athletes
Disordered Eating/ Eating Disorders (DE/ED) - Not all DE/ED involve sufficient or consistent energy restriction to meet criteria for LEA
Energy Availability = the amount of energy available to support the body’s health and function activities once the energy committed to exercise has been subtracted from dietary energy intake.
= (Energy intake - Energy cost of exercise)/Fat free mass
Low Energy Availability occurs when there is a mis-match between energy intake and exercise load, leaving insufficient energy to cover the body’s other needs. This may lead to a decrease in metabolic rate and reduction in activity of many body systems, and underpins the Relative Energy Deficiency in Sport (RED-S) syndrome.
The DSM-5 recognises the following ED:
- Anorexia Nervosa
- Bulimia Nervose
- Binge Eating Disorder
- Other specified feeding and eating disorders
- Avoidant/Restrictive Food Intake Disorder
References
Mountjoy et al. IOC Consensus Statement on Relative Energy Deficiency in Sport (RED-S): 2018 Update. Int J Sport Nutr Exerc Metab. 2018; 28(4):316-331
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association, 2013.
Inappropriate eating practices can have detrimental effects on sports performance. In addition to the direct impairment of physiological and psychological function, DE can increase the risk of illness and injury, compromise training quality and consistency and indirectly interfere with competition goals.
When starved of energy, the body responds by reducing its metabolic rate. Since the human brain operates at a very high metabolic rate, and uses a substantial portion of total energy and nutrient intake, the brain is particularly vulnerable to inadequate fuel for its brain function. A person with DE may struggle to make decisions, solve problems and regulate their emotions. Restricted eating, malnourishment, and excessive weight loss can lead to changes in brain chemistry, resulting in increased symptoms of depression and anxiety.
All of these may affect the athlete’s performance, their ability to engage in day-to-day tasks, their capacity for insight into problems associated with their eating, and their ability to engage with psychological treatments.
Three categories of sports, defined as aesthetically judged, gravitational and weight class, are consistently identified as high risk for the development of DE and EDs. Successful performance in these sports generally involves individual, or combinations of, features such as low body mass, leanness, high power to weight ratio, subjective judgements on appearance and rapid weight loss for weigh-ins. It should be remembered however that athletes are at risk of DE and ED across all sports and these high-risk categories are neither exclusive nor exhaustive.
Weight sensitive sport categories | Examples |
|---|---|
Aesthetically judged sports | Rhythmic and artistic gymnastics, figure skating, dancing, diving, body building, cheerleading and synchronised swimming. |
Gravitational sports (higher bodyweight may restrict performance because moving body against gravity is an essential part of the sport) | Long distance running, cross-country skiing, road cycling, mountain biking, ski jumping and jumps events in athletics. |
Weight class sports | Horse racing (jockeys), lightweight rowing, weightlifting, and combat sports such as wrestling, martial arts (judo, taekwondo) and boxing |
Everyone in the high performance sports system has a role as early identifiers of disordered eating. Education and literacy is required around risk factors, warning signs and red flags.
Experiencing an eating disorder
Jessica Smith OAM is a former elite para-swimmer who represented Australia at the 2004 Athens Paralympic Games. Jessica lived with an eating disorder for the majority of her international swimming career and is now an advocate for positive body image, dedicating her life to raising awareness around diversity and disability.
“I battled with an eating disorder for the entirety of my swimming career”.
Contact
For more information please contact disorderedeating@ausport.gov.au